As travel increases and humans continue to expand their presence throughout the world, dermatologists must be familiar with a number of creatures capable of inflicting medically significant injury.
This post describes those creatures which, when encountered by the unsuspecting human, may result in notable morbidity and mortality, or unfavorable skin conditions.
When you’re out and about, you may end up with a few insect bites that can seem scary, and some just might be. We’re breaking down some insect bites and stings to be aware of.
Hymenoptera are the most common cause of insect stings. Most hymenoptera are social creatures that build nests or hives. Hymenoptera stings usually occur in self-defense, when the insect is swatted or stepped on.
If the hive or colony is disturbed, hundreds to thousands of stings may follow. Medically significant hymnoptera will be discussed below and include apidae (honey and bumblebees), vespidae (wasps, hornets, yellow jackets, paper wasps), and formicidae (imported fire ants).

The stinging apparatus of apidae and vespidae is connected to a venom-filled sac. In honey and bumblebees, the barbed stinger and venom sac detach following contact, resulting in death of the insect. The barbed stingers of bees should be removed immediately to prevent further release of venom and potential foreign body reaction.
Hornets and wasps, on the other hand, are able to sting multiple times as their stinger does not detach.
The resultant injury sustained by apidae and vespidae stings ranges from mild local reactions to systemic reactions including anaphylaxis. The venom of bees, hornets, and wasps, contains phospholipase A which is thought to be responsible for IgE sensitization. Local reactions to bee, hornet, or wasp stings commonly manifest as painful, papular urticaria which develops within minutes and typically resolves within hours to days.
In large local reactions, the pruritus, erythema, edema may spread to encompass a more extensive area (over 10 cm), peaking at 24-48 hours before resolving. Those who experience large local reactions may develop similar reactions upon subsequent exposure to the same insect. Additionally, in these patients, there is an approximate 5-15% risk of anaphylaxis with subsequent stings. Reactions limited to the skin may be symptomatically treated with cold compresses, antihistamines, non-steroidal anti-inflammatory drugs, and high potency topical corticosteroids.
Oral corticosteroids may be required for large local reactions and immunotherapy may be considered to reduce the risk of future stings.
Toxic systemic reactions to vespids may result when a large number of stings is sustained. Although clinically similar to an allergic reaction, toxic systemic reactions due to multiple stings are caused by the vasoactive constituents of the venom rather than an allergic mechanism, and radioallergosorbent testing, which detects allergen-specific IgE antibodies in the serum suggesting an allergic reaction, is recommended to distinguish the etiology.
Anaphylaxis, a type I IgE-mediated hypersensitivity reaction, is estimated to occur in 1.5-34% of patients sustaining an insect sting. Those at increased risk for severe systemic reactions include those with increased age, prior venom sensitization, underlying cardiovascular disease, and patients with mastocytosis. Symptoms of anaphylaxis may occur as early as 10 minutes or as late as 72 hours after the sting. Early signs and symptoms include generalized urticaria, angioedema, and flushing, and may progress to bronchoconstriction, laryngeal edema manifesting as wheezing, hypotension, cardiovascular collapse, and, potentially, death.
Elevated concentrations of serum histamine, tryptase, and mast cells support the diagnosis of anaphylaxis. Immediate intramuscular epinephrine is the initial acute treatment and patients should be discharged with a prescription for an epinephrine auto-injector and clear instructions for use as well as an allergy identification bracelet.
Additionally, all patients with systemic reactions should be referred to an allergist for skin prick or serum immunoassays to confirm venom-specific IgE as well as venom immunotherapy which is available for both honeybee and vespid allergies. Venom immunotherapy is highly effective and has been demonstrated to lower the risk of a subsequent systemic allergic reaction from 30-60% to less than 5%.
Imported fire ants (Solenopsis invicta and Solenopsis richteri) are believed to have been imported from South America via ship to Mobile, Alabama in the 1950s with subsequent spread throughout the southern United States. They are also found in regions of Mexico, the Caribbean, New Zealand, Australia, Taiwan, and China.
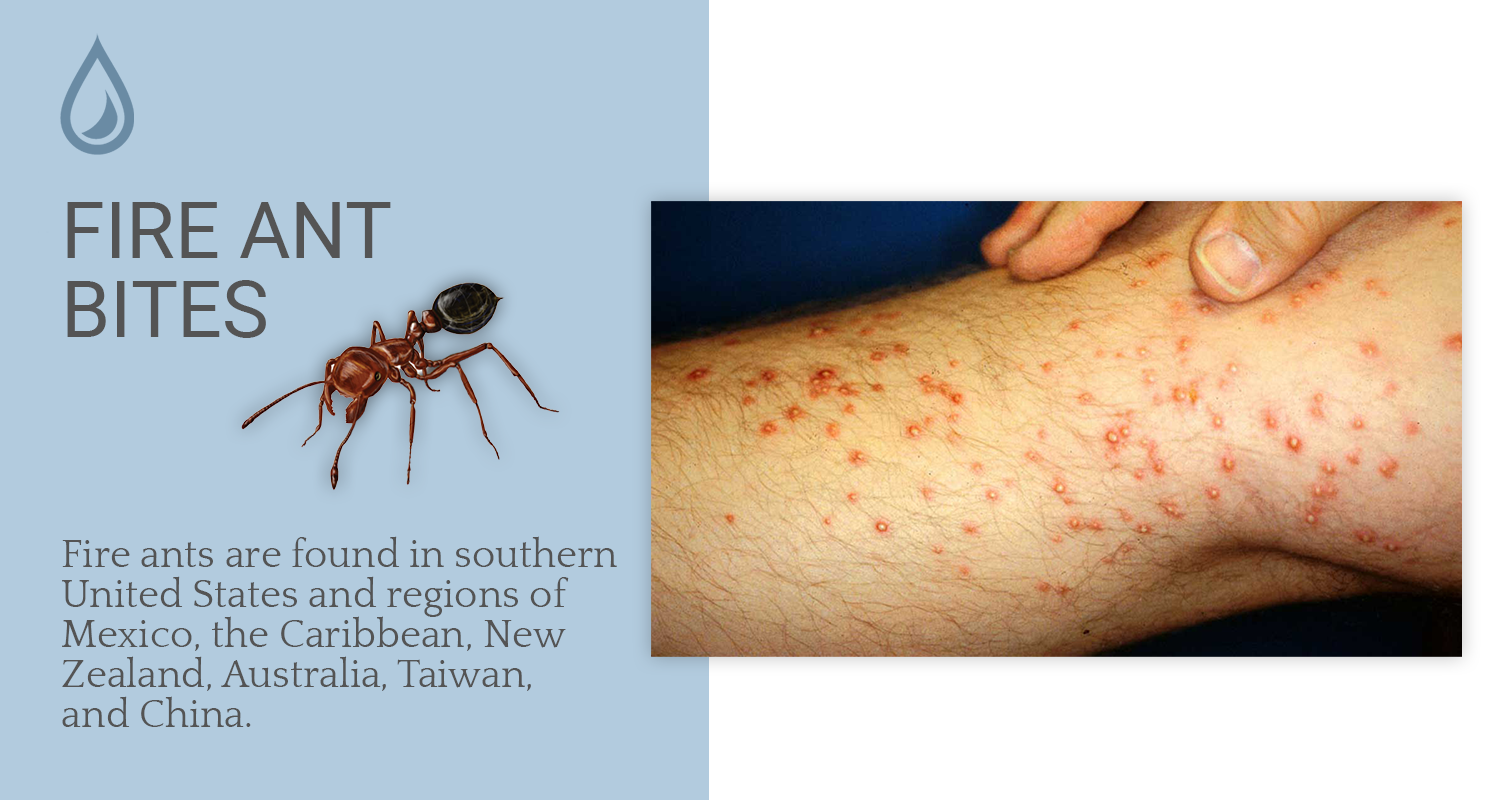
In endemic areas, they are the leading cause of hymenoptera hypersensitivity reactions. Fire ants are notoriously difficult to avoid.
In fact, one study revealed that more than 50% of people fall victim to the sting of this aggressive creature within 3 weeks of moving to an endemic area. Fire ants typically live in mounds proportional to the size of the colony.
When disturbed, the ants stream out of the mound in a swarm, stinging anything they encounter including both humans and animals. During times of flooding, these resourceful insects have been observed to self-assemble into waterproof rafts to avoid drowning. These “ant rafts” may float into houses where they may subsequently inflict stings on the inhabitants.
Equipped with a stinging apparatus located on the distal tip of the abdomen, fire ants are capable of inflicting multiple stings within a brief period of time. After grasping the skin with their mandibles, they sting while pivoting their body in a circular pattern. They should be removed promptly to prevent further injury. In those who are immobile such as nursing home patients or infants, dramatic reports exist of massive attacks in which ants were found completely covering the victims resulting in death in some cases due to cardiovascular or respiratory collapse or anaphylaxis.
The venom of fire ants is composed of predominantly of water-insoluble piperidine alkaloids, responsible for the formation of sterile pustules. The remainder of the venom consists of allergenic proteins, Sol i I-IV, which may cross-react to the venoms of honeybees, yellow jackets, and the centipede Centuroides vittacus.
The sting of the fire ant results in varying clinical presentations ranging from local reactions to life-threatening anyphylaxis. Local reactions are characterized by a wheal and flare reaction with intense burning sensation. In the majority of cases, characteristic sterile pustules develop within 24 hours. Large local reactions are notable for expanding erythema and edema contiguous with the sting site which may persist for 2-3 days. The sequelae of a massive attack is due to a toxic reaction to the hemolytic, cytotoxic, neurotoxic properties of the venom.
Anaphylaxis may occur in up to 1% of those who are stung and may result from a single fire ant sting.
Local reactions may be treated with topical corticosteroids and oral antihistamines. Allergic patients should be provided with an allergy identification bracelet and an epinephrine auto-injector and proper instructions for use. Furthermore, referral to an allergist for appropriate diagnostic studies and immunotherapy is vital to prevent another potentially life-threatening anaphylactic event.
Confirmation of an allergy to fire ant venom may be accomplished by skin-prick testing or serum testing for the presence to venom-specific immunoglobulin E antibodies. Fire ant whole body extract is used for immunotherapy with conventional protocols that may last 3 to 6 months or more and comprise 25 to 28 injections to reach the mainteance dose. Recent studies have demonstrated the efficacy of rushed one-day protocols in which 10 injections are given during the course of one day with maintenance dosing commencing on day 8.
While not everyone’s favorite to face and look at, it’s important to understand arachnids and the dangers of certain bites.
Armed with venom that is nontoxic to mammals and mouthparts too small or weak to pierce human skin, the vast majority of arachnids are harmless to humans. The spiders most likely to pose a medical risk to humans include the black widow, the brown recluse, the Australian funnel-web spider, and the South American armed spider.
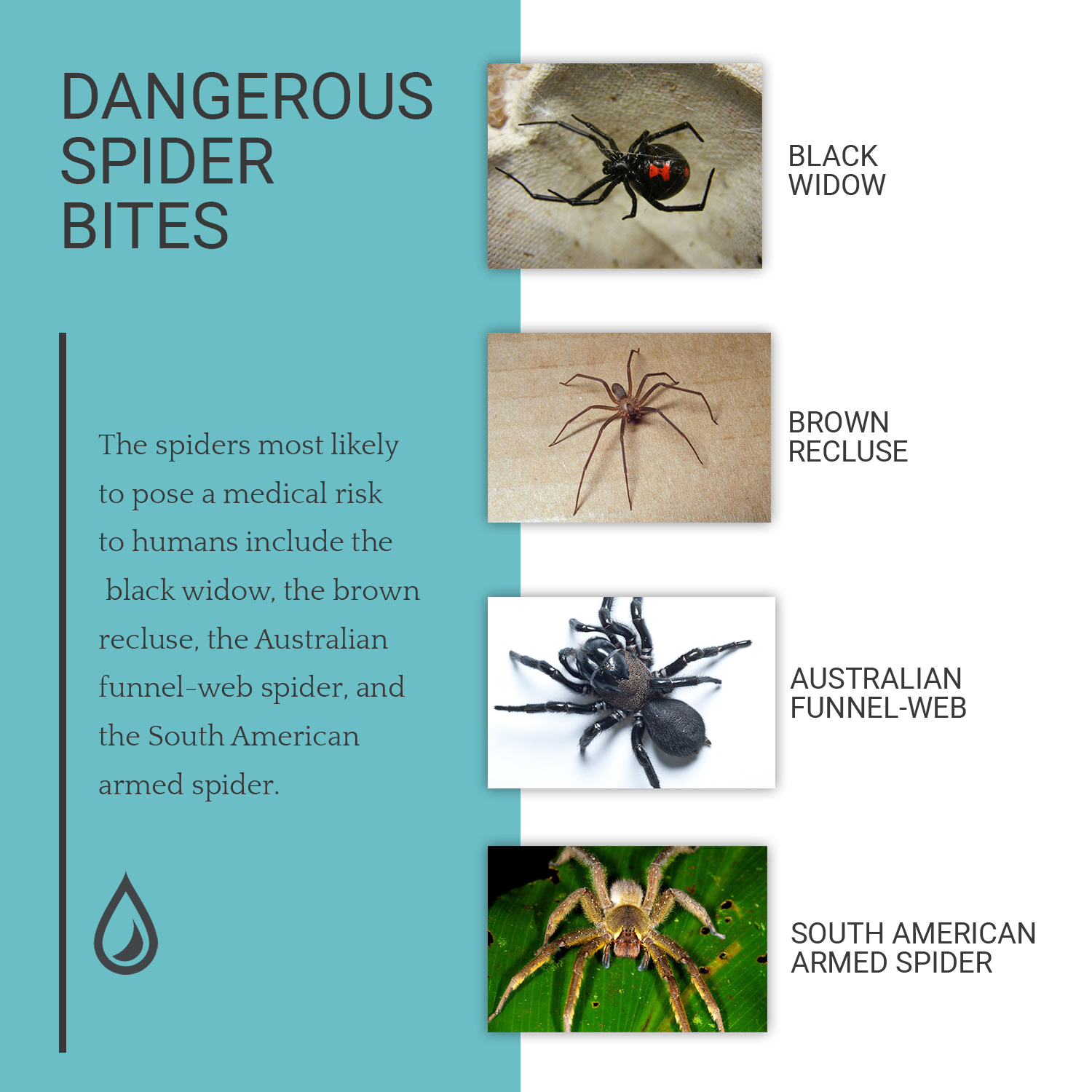
Black Widow Bites
The black widow spider (Latrodectus species) is found throughout tropical and temperate latitudes worldwide. In the U.S., it is predominantly found in the southern and western states under stones, within woodpiles, or in outhouses. The black widow spider is characterized by a glossy, black body with a red hourglass on its abdomen. Although males may bite, it is only the female black widow that is capable of significant envenomation. A bite by a black widow spider may result in local erythema and pain.
Black widow venom, alpha-latrotoxin, is a neurotoxin that causes the presynaptic release of autonomic neurotransmitters resulting in the rapid onset of systemic symptoms including nausea, vomiting, diaphoresis, agitation, hypertension, and muscle cramping. Abdominal rigidity may mimic an acute abdomen. In rare cases, myositis, priapism, respiratory arrest, and death may occur.
Treatment includes local wound care, ice, elevation, and immobilization. Tetanus prophylaxis should be given following all envenoming spider bites as Clostridium tetani spores and bacteria are commonly found throughout the environment and may gain entrace to the body via abrasions and wounds. Muscle relaxants and analgesics are often used for black widow bites. Equine-derived antivenom may be employed for severe systemic cases, however, symptoms may subside spontaneously within hours to days. Furthermore, antivenin has been associated with immediate hypersensitivity reactions anaphylaxis, and may produce serum sickness 1-2 weeks following administration in up to 75% of patients. Its use is recommended in those cases involving patients with marked systemic symptoms unresponsive to other measures. It should be used only in locations where anaphylaxis may be adequately treated.
Brown Recluse Bites
The brown recluse spider (Loxosceles spp.) is found in North and South American. In the U.S., the brown recluse predominantly inhabits the south-central United States. It is identified by its brown color, and in females, a characteristic darker brown violin-shaped marking on the dorsal cephalothorax. The bite of the brown recluse may result in necrotic skin lesions due to venom containing sphingomyelinase D and hyaluronidase. The platelet aggregation, dermatonecrosis, and hemolysis caused by sphingomyelinase D is felt to result in cutaneous ulceration and systemic effects.
Hyaluronidase may increase the spread of the lesion. The bite itself may go unnoticed and commonly occurs when the spider is trapped between bedsheets or clothing and the skin of the victim. The majority of cases are self-limited with mild erythema and edema and heal spontaneously without supportive care. In cases of dermatonecrotic loxoscelism, initially, a dark macule with surrounding erythema may appear, progressing within hours to cyanosis with a central vesicle or bulla.
During the following weeks, a thick eschar gradually forms and then falls off to reveal a necrotic ulcer. A small minority of patients may experience systemic reactions including hemolysis, renal failure, and disseminated intravascular coagulation.
Treatment includes cleaning the wound, compression, ice, elevation, analgesics, and tetanus prophylaxis. The use of dapsone has been demonstrated to be ineffective. Furthermore, it carries the risk of methemoglobinemia, and in those who are glucose-6-phosphate dehydrogenase (G6PD) deficient severe hemolysis may occur due to oxidative denaturation of hemoglobin which G6PD normally prevents.
Early excision and intralesional corticosteroids are contraindicated as these measures may result in more tissue damage than conservative treatment. Healing may take several weeks to occur and excision and grafting may be considered for chronic ulcers 6 to 8 weeks after the initial injury.
Australian Funnel-Web Spider Bites
Internationally, the Australian funnel-web spider (Atrax and Hadronyche spp.) is considered the most lethal spider in the world. It resides in southeastern and coastal Australia. Although cases of envenomation are rare, the Australian funnel spider bite remains a relevant medical entity given its life-threatening nature and the availability of an effective antivenom. The spiders are large (4 cm long) and aggressive. The bite of the Australian funnel spider is remarkable for visible puncture wounds created by long, sturdy fangs up to 5 mm in length capable of piercing fingernails.
Cases of mild envenomation with its venom, the neurotoxin δ-atracotoxin, may yield local paresthesias, numbness, and spasms while severe envenomation results in autonomic and neuromuscular excitability with initial hypertension, tachycardia, diaphoresis and nausea progressing to bradycardia, hypotension, respiratory edema, and in some cases, coma. Deaths have been reported to occur within 15 minutes in children. Treatment consists of application of a pressure immobilization dressing until the administration of antivenom, a purified IgG derived from rabbits hyperimmunized with Atrax venom.
The South American Armed Spider Bites
The South American armed spider (Phoneutria spp.), as its name suggests, is found in South America as well as Central America. A large spider with a body reaching up to 5 cm in length, it often resides in banana clusters. When threatened, it raises its front legs, displays its fangs, and bristles its arm hairs. Armed spider venom, containing the neurotoxin, PhTx-3, targets both the peripheral and central nervous systems.
In the majority of cases, the bite of the spider may result in local effects such as extreme pain, piloerection, and diaphoresis at the bite site. Systemic effects are less common and may include hypertension, tachycardia, nausea, vomiting, priaprism, increased salivation, vertigo, and in rare cases, death. The treatment of armed spider bites should include tetanus prophylaxis, elevation and immobilization of the involved extremity, and analgesics. Following antivenom skin testing, the equine-derived antivenom may be administered.
It is important to keep in mind that the majority of presumed spider bites are in fact caused by another etiology. A definitive diagnosis of a spider bite may be made only if the spider was observed inflicting the bite and then subsequently captured and positively identified by an expert entomologist. The differential diagnosis includes infections (MRSA, herpes, erythema migrans), vasculitis, other arthropod bites, urticaria, and contact dermatitis.
Multiple bites or bites simultaneously sustained by multiple members of the same household should cast in doubt the diagnosis of a spider bite.
Scorpions are characterized by their large claws, four pairs of legs, and segmented tail which ends in a venom-containing stinger. Globally, scorpions are a significant cause of morbidity and mortality. Of the roughly 1500 species of scorpions found worldwide, approximately 30 pose a health threat to humans. The South American Buthidae is considered the most dangerous family of scorpions worldwide. Of the approximately 70 species of scorpion found in North America, only the genus Centuroides, which resides in the southwest US and Mexico, is considered to be medically important]. However, as international travel has increased, cases of envenomation by non-endemic scorpions inadvertently transported to the US have been reported.
Stings occur when the victim encounters a scorpion hidden in shoes, under sleeping bags, in closets, cellars, or woodpiles. Neurotoxic peptides are the main active component of venom from dangerous scorpions occurring at varying levels depending on the species.
The severity of a scorpion hinges on the species involved and may range from a mild local reaction comparable to a bee sting to a life-threatening systemic reaction due to activation of both the sympathetic and parasympathetic nervous systems. Children and the elderly are at a higher risk of developing respiratory, cardiovascular, and neurologic complications.
In severe envenomations, the evolution of symptoms is rapid. Following the initial sting, pain may be accompanied first by a cholinergic stage (bradycardia, hypotension, nausea, emesis, diaphoresis, increased salivation, nystagmus, and priapism), then followed by an adrenergic stage (hypertension, tachycardia, tachypnea, dyspnea, agitation). It has been noted that the presence of gastrointestinal symptoms may be a harbinger of a more severe course and vigilance is recommended. Potentially lethal envenomation may lead to cardiovascular collapse and pulmonary edema.
Management consists of local wound care and pain management as well as tetanus prophylaxis when indicated. Cases of systemic involvement may necessitate supportive therapy and immediate administration of antivenom where available. Anaphylaxis and serum sickness are potential complications of antivenom treatment. Studies have also demonstrated benefit of prazosin via blockade of alpha-1 receptors in reversing the cardiovascular manifestations.
Inhabitants of tropical and subtropical regions, Chiropods, or centipedes, are fast-moving, aggressive arthropods. These nocturnal creatures are characterized by a long, segmented body with pairs of legs attached to all but the final segment (Figure 15.8). Modified appendages which are attached to the first segment act as claws and are capable of releasing venom through specialized ducts.
The most dangerous centipede is of the Scolopendra genus which may reach a length of 30 cm. They are found worldwide in temperate and tropical zones; in the United States, they are found predominantly in the southern states and Hawaii.
Centipede venom has been found to contain several enzymes including metalloproteinases and hyaluronidases, as well as non-enzymatic toxins (neurotoxins, cardiotoxins, and myotoxins). A bite may result in excruciating pain, pruritus, erythema, edema, and bleeding, but is generally self-resolving with no serious morbidity or mortality. However, there are case reports of centipede stings causing necrosis, myocardial infarction, proteinuria, rhabdomyolysis with renal failure, Well’s syndrome, and toxicity following ingestion.
Treatment includes local wound care and pain management. Pain control may be achieved with ice packs, hot water immersion, local anesthetics, and oral analgesics. Antihistamines and topical and/or systemic corticosteroids may be employed, and antibiotics may be administered as needed for secondary bacterial infection. Tetanus prophylaxis is recommended.
Diplopods, or millipedes, differ from centipedes in that they have two pairs of legs attached to each segment of their bodies. They are vegetarians and are not known to bite humans. When disturbed, they release noxious substances such as benzoquinone, hydroquinone, and hydrogen cyanide (normally?) secreted by repugnatorial glands along the length of their body[56]. In the majority of species, these substances exude from these glands. However, some species are capable of squirting the substance up to 25cm.
Cutaneous exposure results in a prickling or burning sensation with or without paresthesias that may progress to vesiculation. A characteristic mahogany discoloration develops simulating cyanosis, necrosis, or gangrene. This discoloration occurs due to oxidation of quinones and may persist for months. Treatment includes profuse irrigation to remove the toxins, analgesics, and topical corticosteroids.
Worldwide, it is estimated that almost 200,000 people die each year of snake bites. However this may be an underestimate due to lack of reporting in much of the developing world.
According to the 2010 American Association of Poison Control Centers, there were over 3,000 reports of venomous snake bites treated in medical facilities in the United States. Snakes use their venom to immobilize their prey and as self-defense when threatened or provoked. Of the 3000 species of snakes found globally, approximately 15% are venomous, all of which are found in four families: Atractaspididae, Colubridae, Elapidae, and Viperidae.
The venomous snakes indigenous to North America are confined to the Elapidae and Viperidae families which will be discussed below.
Rattlesnakes, copperheads, and water moccasins, members of the subclass Crotalinae of the family Viperidae, are responsible for the majority of venomous snake bites in the U.S. This group of snakes is commonly referred to as pit vipers owing to the infrared heat-sensing pits located posterior to the nostrils. Other characteristic features include prominent fangs, elliptical pupils, and triangular-shaped heads. With the exception of Maine, Alaska, and Hawaii, rattlesnakes inhabit all states of the continental U.S. Copperheads are found predominantly in the eastern U.S., and water moccasins are native to the southeastern U.S.
The spectrum of clinical presentations due to crotalid envenomation may range from local reactions to fatal systemic reactions. Severity is dependent on the age and underlying health of the victim, the location of the bite, and the amount of venom injected. Interestingly, approximately 25% of crotalid bites are “dry”, meaning that no venom was injected.
Furthermore, the components of the venom may vary according to season, as well as the age and nutritional status of the snake. Crotalid envenomation commonly results in immediate pain and the appearance of one or two fang puncture marks. Within the hours, erythema, edema, bullae, eccchymosis, lymphangitis, and lymphadenopathy may develop. Associated nonspecific systemic symptoms may include nausea, emesis, lethargy, weakness, and diaphoresis.
Patients should be closely monitored for the development of more severe systemic manifestations including hypotension, tachycardia, compartment syndrome, rhabdomyolysis with renal toxicity, and disseminated intravascular coagulation. Neurotoxicity is rare in crotalid envenomation except in bites caused by the Mohave rattlesnake.
Treatment begins in the field and includes removing the victim from the vicinity of the snake and immediately transporting the victim to the nearest health care facility.
An attempt to capture the snake for identification purposes is discouraged owing to the risk of creating another victim. Instead, a photo may be taken from a safe distance if possible. Due to the risk of increased morbidity, several dangerous practices should be avoided including incising and suctioning venom from the wound, cryotherapy, electrotherapy, and applying a tourniquet.
Wound management includes thoroughly cleaning the area, repeated circumferential measurement along the affected limb, gentle immobilization, elevation of the limb, and administration of analgesics and tetanus prophylaxis as needed. Serial neurologic exams should be performed hourly until the edema resolves. Laboratory studies should be performed to evaluate for the development of coagulopathy and rhabdomyolysis. Fasciotomy should be reserved for compartment syndrome that does not resolve after the administration of anti-venom.
Candidates for anti-venom therapy include those with progressive worsening of local injury, coagulopathy, or systemic manifestations. An ovine-derived anti-venom, Crotalidae Polyvalent Immune Fab is currently available in the United States and is infused four times over a period of 18 hours. It is associated with acute hypersensitivity reactions in 16% and serum sickness in 14.1%.
Elapidae, or coral snakes, are found primarily in Florida and Texas. Although coral snake envenomation is much less common that crotalid envenomation, deaths have been reported and neurotoxicity is characteristic.
Venomous coral snakes are notable for their distinctive red, yellow, and black stripes. They can be distinguished from non-venomous species which display alternating red and black banding recalled by the colloquialism: “Red and yellow, kill a fellow. Red and black, venom lack”. Unlike crotalids, coral snakes lack long fangs. Instead, they have small rows of teeth, and upon biting a victim, must gnaw the skin in order to pierce it and deliver venom.
Unlike crotalid envenomation, significant local tissue injury and coagulopathy are not characteristic of coral snake envenomations. Instead, the site of the bite may be erythematous with mild edema and pain. In further contrast, the victim may demonstrate neurological manifestations ranging from mental status changes, tremors, and hypersalivation to obtundation and respiratory paralysis necessitating ventilatory support. It is important to note that the onset of neurologic effects may be delayed for up to 24 hours.
Field treatment is similar to that of crotalids with emphasis placed on transporting the victim immediately to the closest medical facility.
Tetanus prophylaxis should be administered as appropriate. Serial neurologic and cardiorespiratory evaluation should be conducted with intubation and mechanical ventilation if needed. In confirmed coral snake envenomations, North American elapidae anti-venom, if available, should be administered immediately.
Derived from horse serum, North American anti-venom may cause an acute hypersensitivity reaction and serum sickness. If anti-venom is not available, respiratory support should result in complete recovery in the majority of patients. However, the duration of mechanical ventilation may be as long as one week.
Harmful bites and stings aren’t just for land animals. Let’s dive into some marine creatures you have to keep an eye out for when splashing away.
Jellyfish are members of the phylum Cnidaria. Of the approximately 9000 species of Cnidaria, at least 100 pose a threat to humans. There are three classes of Cnidaria which are hazardous to humans. The first, the Scyphozoans, or “true” jellyfish, are characterized by tentacles which are arranged radially at regular intervals around and within the bell.
The second, and most deadly class, the Cubozoans, or “box” jellyfish, are distinguished by tentacles arising only from the corners of their box or cube shaped bells. The Cubozoans comprise two subgroups containing the Carybdeids and the Chiropods. The Carybdeids include the Hawaiian box jelly fish and Carukia barnesi, the small jellyfish responsible for “Irukandji Syndrome”. The Chiropods include Chironex fleckeri, the Australian sea wasp, considered the most dangerous animals in the world.
The third class, the Hydrozoa (“other” jellyfish), includes the Physalia species and the Gonionemus found in the Sea of Japan.
Jellyfish are armed with stinging cells, or nematocysts, which contain venom and are triggered upon chemical or physical stimuli. Nematocysts are capable of stinging even after the jellyfish is dead or when the tentacles are separated from the jellyfish. Venom is delivered to small dermal capillaries and dermal tissue, where it is thought to be absorbed systemically via the lymphatic system. The venom contains both toxic and antigenic properties that are dermatonecrotic, cardiopathic, hemolytic, or neurotoxic.
The majority of reactions to jellyfish are localized.
However, systemic and fatal reactions may occur. The severity of the reaction is dependent on the size, age, and underlying health of the victim, the body surface area involved, the number of nematocysts discharged, and the toxicity of the venom.
Localized cutaneous lesions appear as linear, urticarial erythema which may progress within minutes to hours to vesiculation and sometimes necrosis in the area of contact with tentacles.
Pain, burning sensation, paresthesias, and hyperhidrosis may accompany the skin lesions. Cases of recurrent eruptions occurring at variable intervals after the initial injury have been reported.
Systemic symptoms may accompany the cutaneous manifestations of a jellyfish sting and include local cramping and muscle spasms, paresthesias, nausea and vomiting, weakness, dizziness, and malaise. The Irukandji syndrome, named after the aboriginal Australian tribe who inhabit Northeast Queensland, was first described in 1952. Barnes positively identified the culpable jellyfish, which came to be known as Carukia barnesi, by envenomating himself, his 9-year-old son, and a local lifeguard in 1961. Carukia barnesi is a small jellyfish characterized by four tentacles and a bell of approximately 2 cm. Approximately 20-30 minutes after a relatively innocuous sting, victims experience severe, cramping pain, nausea, vomiting, diaphoresis, shortness of breath, and a sense of impending doom.
Massive catecholamine release is thought to be responsible. The majority of envenomations resolve spontaneously. However, cases of heart failure, pulmonary edema, and hypertensive stroke necessitating supportive therapy have been reported as well as death. Various reports of Irukandji-like syndromes have been described in Thailand, Hawaii, and Florida.
Death due to jellyfish envenomation may occur from anaphylaxis or as a result of exposure to toxins. Potentially life-threatening envenomation may result from contact with Chironex fleckeri (the Australian box jellyfish or sea wasp) a large bell-shaped creature whose bell may span up to 30 cm and whose long tentacles may span up to several meters. Its potent venom contains dermatonecrotic factors and cardiotoxins. It is believed that approximately 10 cm of tentacles are sufficient to deliver a fatal dose. Contact with the Australian box jelly may results in whip or ladder-like cutaneous lesions, and in some cases, death from cardiovascular collapse within minutes.
Management of all jellyfish stings should include removing the victim from water to prevent drowning with assessment of the victim and initiation of basic life support as needed. Steps should be taken to prevent further stinging by non-discharged nematocysts. The sting should not be rubbed or rinsed with fresh water due to the danger of massive nematocyst discharge. Different species respond differently to various treatments, and it is important to note that vinegar (3-6% acetic acid) effectively inhibits nematocyst discharge in some jellyfish, but may trigger discharge in other species[83]. The Australian Resuscitation Council recommends vinegar use for the Australian box jellyfish and for cases of Irukandji syndrome. If vinegar is not available, seawater may be used to rinse the sting. There is no evidence supporting the use of urine in the treatment of jellyfish stings. Once nematocysts are deactivated, all remaining tentacles should be removed from the victim.
Although inactivation of further nematocyst firing is critical, it does not provide pain relief for venom that has already been injected. Following removal of remaining tentacles, hot water may be applied to the area for pain relief and denaturing of venom.
Localized reactions may then be symptomatically treated with antihistamines, topical corticosteroids, and local anesthetics. Tetanus prophylaxis should be administered, if indicated.
Systemic reactions secondary to Irukandji syndrome may require analgesics, oxygen, antiemetics, and supportive treatment as necessary. The toxic effects of envenomation by Chironex fleckeri may be neutralized by antivenom which is composed of immunoglobulins from hyperimmunized sheep serum. It should be administered in cases of severe pain, dyspnea, dysphagia, dysphonia, unconsciousness, cardiorespiratory arrest, hypotension, or dysrhythmia. Basic or advanced life support and intensive care measures should be taken as appropriate.
Found in all oceans, sea urchins belong to the phylum Echinodermata which also includes sea cucumbers and starfish. Sea urchins are slow-moving, coastal dwellers with numerous spines. Depending on the species of sea urchin, the spines may be sharp or blunt, solid or hollow, and may or may not be venomous. Most venomous species are found in tropical and subtropical regions. The flower sea urchin (Toxopneustes pileolus), found off the coast of Japan, is the most venomous sea urchin known.
Most injuries from sea urchins occur when the brittle calcium carbonate spines break off and become embedded in the skin when accidentally stepped on or handled. Penetration injury results in localized sharp pain, bleeding, erythema, and edema. Arthritis, synovitis, or tenosynovitis may occur if the injury is periarticular. The pigment of the implanted spines may leave behind a purple or black tattoo.
The affected area should be soaked in hot water (as hot as the patient can tolerate) to deactivate toxins and alleviate pain. Tetanus prophylaxis should be administered.
Although spine fragments may be absorbed by the body within 1 to 3 weeks, an attempt to remove all embedded fragments should be made as infections, granuloma formation, and arthritis may arise from retained spine fragments and the ensuing foreign body reaction .
Removal is often complicated by breakage of the delicate spines, and many techniques have been described using needles, forceps, punch biopsy, and erbium-YAG laser. Imaging studies including plain radiographs, ultrasound, or MRI may be performed to confirm the complete removal of retained spines. Antibiotics are indicated for secondary infections.
Stingrays, members of the class Chondrichthyses, are flat bottom-dwellers that reside in shallow waters, hidden beneath a layer of sand with only their eyes visible. Stingrays may be found in both saltwater (in temperate and tropical coastal regions throughout the world) as well as in fresh or brackish waters (in South America, Southeast Asia, and Africa). I
njuries most frequently occur on the lower extremities when a swimmer or wader inadvertently startles the creature. Injury may be avoided by shuffling one’s feet when walking in shallow water, alerting the stingray of human presence, and giving it ample time to swim away. When provoked, the stingray’s whip-like tail swings forward impaling the victim with serrated spines which range in size from less than 2.5cm to over 30 cm in length and release a heat-labile, vasoconstrictive venom. The immediate effects are local, severe pain out of proportion to the injury and vasoconstriction progressing to necrosis of the involved area. Systemic effects may include myocardial infarction, cardiovascular arrhythmias, and bradycardia. Rarely, death may occur from penetration injuries to the thorax or abdomen.
Treatment consists of irrigating the area with hot water to inactivate the venom and administering local anesthetic or a nerve block without epinephrine as well as parenteral analgesics. Tetanus prophylaxis should be given. The wound should be debrided and explored for retained spines. If superficially located, the spine should be removed. However, if the spine is found to be penetrating the neck, thorax, or abdomen, or completely though an extremity, it is best left in place until the patient is taken to a medical facility where this can be performed safely.
Radiographic studies may be employed to ensure complete removal. Secondary infections by gram negative (Vibrio) and gram positive (Staphylococcus and Streptococcus) bacteria are common and prophylactic antibiotics are recommended, most commonly a five day course of a quinolone or amoxicillin with clavulanic acid.
All in all, taking precautions around these creatures can help save you the skin damage and potentially worse effects.